Lung cancer and mesothelioma service guidance during the COVID-19 pandemic
At the time of writing, the COVID-19 pandemic is predicted to place unprecedented pressure on the NHS. The trend in the number of deaths reported with COVID-19 infection matches those reported from Italy but lag by 14 days. We therefore anticipate that services and resources will be redirected and adherence to the currently commissioned National Optimal Lung Cancer Pathway will be impossible. It is important that measures are taken to preserve cancer services throughout the pandemic, but in a manner that balances first, the risks to the cancer patient contracting COVID-19 during investigations and treatments and second, the care providers’ capacity. The purpose of this guidance is to provide assistance to cancer teams in this regard and in particular to show how pathways can be adjusted to reduce the use of resources and the risk of infection. The guidance also suggests how to prioritise patients most likely to be harmed by delays. The guidance takes further the NHS Clinical Guide for the Management of Patients During the Coronavirus Pandemic (17 March 2020 V1). The guidance also draws on that being produced by the relevant Royal Colleges and specialist societies. This guidance does not cover the Targeted Lung Health Checks and CT screening, currently suspended and awaiting further advice from the National Cancer Programme Team.
This is a rapidly evolving situation and this guidance may need to be updated regularly.
This guidance cannot cover all clinical scenarios. Individual clinicians, trusts and MDTs will always make the final decisions on the most appropriate action for individual patients and their local services.
- Diagnostics and staging
These recommendations are designed to minimise the need for hospital attendance and to minimise the duration of any hospital attendances whilst maintaining an appropriate and effective diagnostic and staging pathway.
- Primary Care clinicians should consider alternative strategies to immediate referral for lower risk patients, supported by risk-prediction tools where available.
- The normal triage process should be employed that includes correspondence with patients; those without cancer, or at very low risk, should not be invited for an appointment at the hospital. Consider telephone consultation and repeat scans for indeterminate findings scheduled after the anticipated reduction in COVID-19 infections.
- Where appropriate, telephone consultations should be used in place of scheduled visits to the hospital, e.g. for results and planning of subsequent tests.
- Ensure that all investigations are necessary to plan treatment; avoid where no treatment is likely.
- Consider whether delaying diagnostic and staging investigations will significantly compromise outcomes before proceeding.
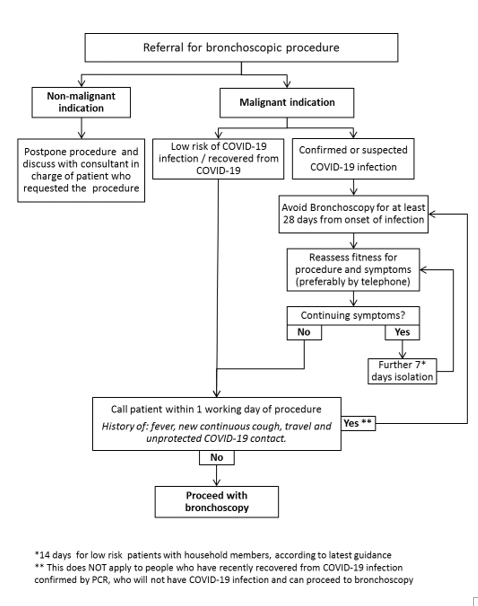
- Follow the guidance for bronchoscopy available on the BTS website / NHSE, (figure 1). In addition:
- Avoid bronchoscopy and EBUS in patients with a low risk of cancer
- Consider interval imaging rather than sampling
- When indicated, use PET-CT prior to any staging EBUS and to identify alternative biopsy target.
- In cases where there is a low risk of mediastinal disease, consider percutaneous lung biopsy or proceeding directly to treatment based on lung cancer probability (including the use of the Herder model)
- Consider day case mediastinoscopy as an alternative to EBUS
- Omit contrast enhanced CT brain in clinical stage II lung cancer.
- Do not perform full lung function testing when the clinician and surgeon are happy with simple spirometry
- Do not perform functional exercise testing in patients with adequate spirometry or if carried out adequate predicted post-operative lung function (ppo-FEV1 and ppo-DLCO >40%) and performance status 0-1
- For patients that do require a functional assessment consider alternatives to a shuttle walk test to minimise number of visits to the hospital e.g. stair climb.
- Consider CT surveillance to measure growth rate rather than staging and treatment in those lesions likely to be indolent or benign, including pure ground-glass nodules and smaller part-solid and solid nodules.
- Prioritise patients with likely aggressive disease or where a delay would result in the patient becoming unresectable.
- Consider implementing virtual nodule management avoiding visits to hospital. Consider extending the scheduling follow-up CTs, in low risk patients well outside the peak of the pandemic. Use telephone follow-up and/or correspondence to convey results.
- In patients with a never/light smoking history and clear radiological suggestion of advanced primary lung cancer, consider plasma test for EGFR mutation instead of biopsy.
Figure 1: Summary of Bronchoscopy Guidelines
- Treatment
Clinicians should discuss with patients whether the risks of starting anticancer treatment could outweigh the benefits during the covid-19 outbreak. This is particularly true for patients considered for systemic anti-cancer treatment (SACT). In the event of disruption to cancer services, surgery, radiotherapy and SACT will be prioritised for patients most in need, according to the Priority Categorisation set out in the NHS Clinical Guide for the Management of Patients During the Coronavirus Pandemic (17 March 2020 V1)
2.1 Surgery and curative-intent treatment
Thoracic surgery capacity has reduced significantly and is likely to reduce further as theatre space and anaesthetic cover is required for additional ventilators. Patients should be offered treatment according to the accepted standard of care until limitations of services require a progressive reduction in surgery. Patients most likely to be harmed by a change of treatment to non-surgical or by a delay in surgery should be prioritised. In addition, radiotherapy services will come under increased pressure so regimes will need adjustment where possible. The MDT needs to discuss this and decide which patients are highest priority. In addition:
2.1.1 Surgery and curative-intent radiotherapy/chemoradiotherapy
- Consider deferring treatment in lesions likely to be indolent, with follow up CT to confirm growth rate.
- Prioritise referral and pathway to thoracic surgery for cases of:
- Symptomatic lung cancer (infection, pain, bleeding, breathlessness)
- Stage IIb/IIIa lung cancer at most risk of stage progression / becoming unresectable
- Plan surgery to minimise length of stay, by using minimal access surgery, day case or day of surgery admission.
- The benefit of adjuvant chemotherapy may be outweighed by the risk so consider omitting this and stopping existing treatment early at 3 cycles.
- In higher risk patients, particularly those not fit for a lobectomy, consider direct referral for radiotherapy.
- Consider treatment without biopsy, as above, using Herder score
- Suspend trimodality treatment for N2 positive lung cancer.
- In patients suitable for SABR without nodal disease and tumours <2cm, consider SABR rather than surgery when surgical capacity is reduced.
- Consider delaying radiotherapy treatment until risk of exposure reduces in patients with stage I-II disease
- Use hypo-fractionated regimens wherever possible- See RCR emergency paper for protocols.
- Consider omitting induction component of chemoradiation and limiting to concurrent therapy.
- Consider temporarily stepping down routine post radical treatment surveillance. An alternative would be nurse led telephone consultations
- Pre- and post-operative clinical appointments should be remote (via secure video-link to telephone call) whenever possible. MDT attendance should be remote (video-link ideally) whenever possible
2.2 Systemic anti-cancer therapy
- Defer face to face consultation with oncologists until complete predictive marker analysis is available.
- Patients should be counselled about the risks of chemotherapy during the pandemic and risk stratified according to tumour biology urgency of treatment.
- Defer treatment of indolent disease.
- Consider restricting SACT to patients of PS 0-1
- Consider offering GCSF to all patients undergoing cytotoxic chemotherapy.
- Utilise the least labour (pharmacist and nursing) intensive regimen where possible e.g. platinum/pemetrexed, taxol/carbo or platinum/oral vinorelbine.
- Use a maximum 4 cycles of cytotoxic chemotherapy per course.
- Denosumab should be available for self-administration.
- Omit routine dental review before commencement.
- Omit maintenance pemetrexed.
- For patients suitable for first-line immunotherapy, monotherapy is preferred over combination chemo-immunotherapy.
- Immunotherapy should be offered 4 or 6 weekly to minimise hospital attendances.
- Third or more line therapy should not to be offered routinely.
- Imaging whilst on treatment should utilise most pragmatic modality- consider CXR rather than CT or alternate between modalities.
2.3 Palliative radiotherapy
- Consider offering radiotherapy without a tissue diagnosis if patient unlikely to benefit from systemic therapy.
- Use hypo-fractionated regimens where possible.
- Omit PCI and thoracic consolidation for ED-SCLC.
2.4 End of treatment
End of treatment summaries should be completed detailing the variation from standard of care to enable subsequent treatment planning.
2.2: Supportive Care
- All patients, regardless of stage, should be offered a discussion regarding advance care planning.
- Enhanced supportive care should be offered to all patients who are stage IIIB/IV.