NLCA State of the Nation 2025: Progress, Pressures and Priorities in Lung Cancer Care
The National Lung Cancer Audit (NLCA) State of the Nation 2025 report has just been published, offering a detailed snapshot of how lung cancer services in England and Wales are performing for patients diagnosed with lung cancer in 2023. The data shows progress in early diagnosis and survival but also flags growing pressures on treatment pathways and persistent inequalities that could slow further progress if left unaddressed.
One of the headline achievements from this year’s report is the record proportion of patients being diagnosed with early-stage disease. In England, 37% of people diagnosed with lung cancer were diagnosed with stage 1 or 2, this was 34% in Wales. This shift in England is likely due to the expanding lung cancer screening programme, which is successfully identifying lung cancers earlier in patients who haven’t yet developed symptoms. Earlier diagnosis is the gateway to curative treatment and better outcomes, so this is a hugely encouraging trend.
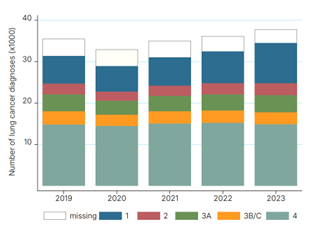
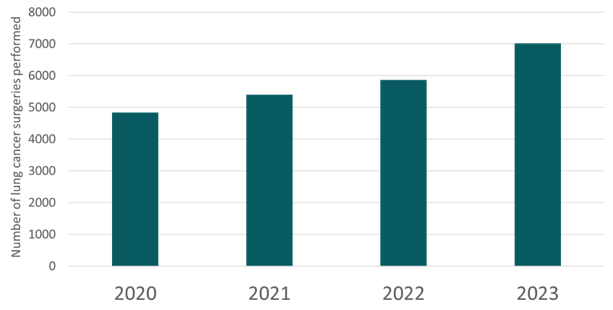
Earlier detection only pays off if it's matched with timely, effective treatment - and here the picture is mixed. Curative treatment rates for early-stage non-small cell lung cancer (NSCLC) remained stable at 80% in England and 77% in Wales. A record number of surgeries were performed in England in 2023 at just over 7,000 lung cancer resections. The proportion of patients with NSCLC having surgery is increasing at 20% in England and 18% in Wales in 2023. With more early cancers being found, surgical capacity will need to grow in parallel to ensure timely delivery, or we risk missing the opportunity for optimal curative treatment.
An area of concern is the time it takes to start treatment. The National Optimal Lung Cancer Pathway for England outlines a pathway from referral to the start of treatment over a maximum of 49 days. For patients with NSCLC, the median time from referral to having surgery was 83 days; only 12% of patients had surgery within the specified time frame of 49 days. In Wales, the median time to surgery was 97 days. These delays matter. They increase patient anxiety, can allow disease to progress and thereby lead to suboptimal treatment options and outcomes. The report makes it clear that as early diagnosis is improving, treatment capacity is struggling to keep up.
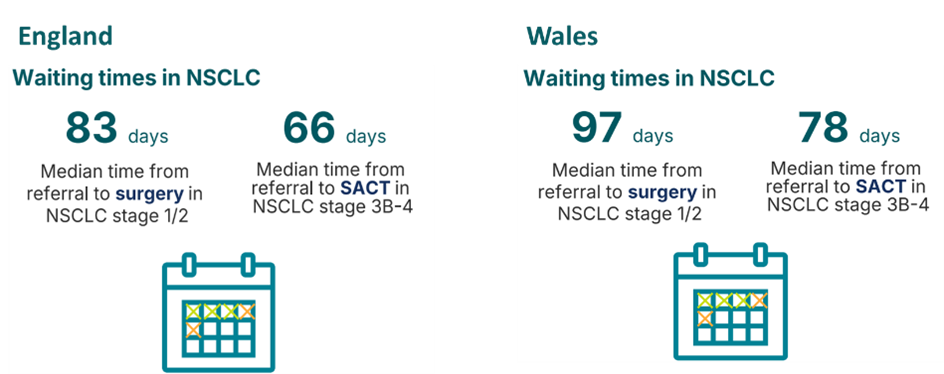
Access to systemic anti-cancer therapy (SACT) for advanced NSCLC also remains uneven. Only 62% of patients in England and 55% of patients in Wales with good performance status (PS 0-1) and advanced stage IIIB-IV disease received SACT in 2023. The NLCA audit standard was met or exceeded by 55 of 124 NHS trusts (44%). Furthermore, the median time between referral and starting SACT for patients with advanced NSCLC was 66 days in England and 78 days in Wales. In an era where immunotherapy and targeted treatments are transforming patient outcomes, this is a critical area for improvement. Faster turnaround times for biomarker testing and better integration of diagnostic and treatment services could help close this gap.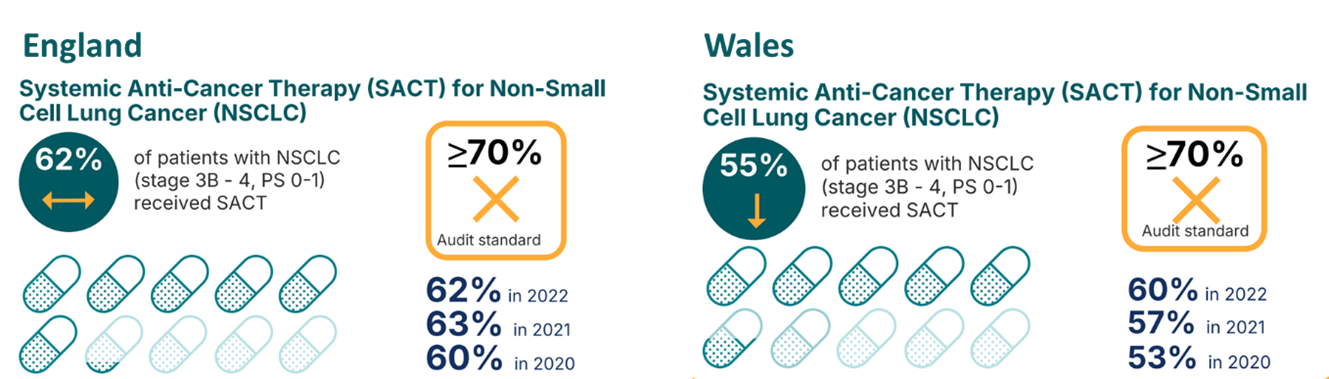
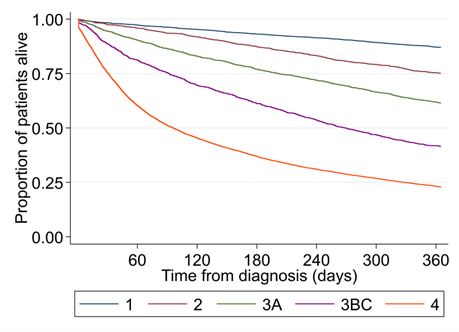
Still, despite these challenges, survival is improving. One-year survival rates are the highest ever recorded by the NLCA - 50% in England and 46% in Wales. That reflects progress in diagnosis, treatment options, and care quality. The improvement in survival is driven by the improved survival in early-stage disease. Stage 4 lung cancer has only seen a 2% increase in one-year survival from 2020 to 2023 (20.8% to 22.8%). Improving SACT treatment rates and survival in advance stage lung cancer must be a priority for the lung cancer community in England and Wales.
Unfortunately, not all the data received by the NLCA was complete enough to report meaningfully. Important aspects of care, such as whether patients had access to a lung cancer nurse specialist (LCNS), or whether their smoking status was recorded, still suffer from poor data completeness. These data items are essential to understanding the full care journey and delivering equitable, personalised support to every patient.
Looking ahead, the NLCA’s 2025 report paints a picture of cautious optimism. We’re diagnosing lung cancer earlier and seeing better survival, however healthcare services are under pressure and capacity must be carefully increased without losing quality of care. If the ambitions of the lung cancer screening programme are to be realised and we want to continue seeing improvements in survival, patients must have a timely experience moving through the lung cancer pathway. We must also improve access to SACT for patients with advanced disease to improve survival for this group. Great progress has been made in lung cancer care over the last few years - what’s needed now is the capacity and commitment to turn that progress into lasting impact and better equitable care for every patient.